Research Article - (2023) Volume 6, Issue 1
Outcome of LCP in Treating Diaphyseal Fractures of Radius and Ulna in Adult Patients
Mushfique Manjur1*, Rafia Afreen Jalil2 and Monaim Hossen32Assistant Professor (Microbiology), Green Life Medical College, Dhaka, Bangladesh
3Professor (Orthopaedics), National Institute of Traumatology and Orthopaedic Rehabilitation, Dhaka, Bangladesh
Received: Mar 13, 2023, Manuscript No. amdhs-23-91477; Editor assigned: Mar 15, 2023, Pre QC No. amdhs-23-91477 (PQ); Reviewed: Mar 23, 2023, QC No. amdhs-23-91477 (Q); Revised: Mar 25, 2023, Manuscript No. amdhs-23-91477 (R); Published: Mar 30, 2023, DOI: 10.5530/ amdhs.2023.1.4
Abstract
Background: LCP can be used in forearm fractures in the conventional plating technique (compression method - principle of absolute stability) for simple transverse or oblique fracture with low soft tissue compromise or in the bridging technique. Locking compression plates have been shown to provide a stronger fixation and perform better than the DCP in older or osteoporotic bone.
Objective: To evaluate the outcome of LCP in treating diaphyseal fractures of radius and ulna in adult patients.
Methods: This prospective observational study was conducted at National Institute of Traumatology and Orthopaedic Rehabilitation from January to December 2018. Patients with diaphyseal fracture of both bone of forearm, aging 50 years and above, were study population. Total 44 cases were included. Clinical, radiological and functional outcome were assessed and followed up for 24 to 30 (Average 25.27 weeks ± 1.39 weeks). Final functional outcome was done with Anderson criteria.
Results: Total 44 patients involved in this study were followed up to one year. Maximum age incidence was found in 51 years-55 years of age. The mean age of the patients was 58.27 years ± 5.68 years ranging from 51 years to 75 years. Out of 44 patients 35 (79.5%) were male and 9 (20.5%) were female. Male to female ratio was 3.86:1. Among 44 cases, 23 (52.3%) had left sided fracture and 21 (47.7%) had right sided fracture. In this study, motor vehicle accident accounted for 23 (52.3%) cases which was the most common cause of injury. Other causes were fall from height in 17 (38.6%) cases and physical assault in 4 (9.1%) in descending order. The mean radiological union time was 12.18 weeks ± 1.53 weeks with 1 case of non-union. Complications were found in 11.4% cases. The mean ROM of flexion-extension and supination-pronation were 133.530 ± 5.440 and 124.410 ± 11.190 respectively at last follow up. The mean Quick DASH score at last follow up was 14.6% ± 7.14%. Out of 44 cases, 22 (50%) were excellent, 21 (47.7%) were good and the remaining 1 (2.3%) was poor.
Conclusion: In concluded, use of LCPs represents an effective treatment in terms of union rate, pain and functional outcomes. The major mechanism of these fractures is Motor vehicle accident. Most common fractures in left-side. In this study, the surgical outcomes were excellent in 50% of cases, 21 (47.7%) were good and the remaining 1 (2.3%) was poor. Internal plating gives good functional results in the treatment of forearm diaphyseal fractures, as long as the surgical technique is perfect.
Keywords
Outcome, Locking Compression Plate (LCP), Fixation of diaphyseal radius-ulna fracture
Introduction
Historically, both bone forearm fractures, like nearly every other orthopaedic injury, were treated with closed manipulation and casting; however, even the best published results of this technique were far from perfect. Evans 1951 reported a series of five patients treated with closed reduction and casting. His technique was reliant upon a tuberosity view radiograph of the proximal radius, which revealed the relative pronation or supination of the proximal fracture fragment. Reduction was thus performed to match the forearm rotation. His results still revealed more than 50 degrees of loss of forearm rotation in more than 30% of patients. Treatment of diaphyseal forearm fractures by open reduction and internal plate fixation is a well-accepted strategy. Open reduction and internal fixation is the first line of treatment and generally accepted as the best method of treatment in adult. Anatomical reduction allows restoration of normal radial and ulnar length to prevent subluxation of proximal or distal radio-ulnar joint and restoration of anatomical alignment essential for normal pronation supination function of the forearm [1]. Diaphyseal forearm bone fractures on the contrary have been reported to be 10 times less frequent than distal radius fractures. The average yearly incidence in adults has been reported to be 1.35 per 10,000 populations, ranging from 0 to 4 per 10,000 populations depending on age and gender. Four-fifths (75%) of forearm shaft fractures occur in children. Above the age of 20, the yearly incidence of forearm shaft fractures remains below 2 per 10,000 people, predominating in males throughout all age groups [2]. Injuries most frequently occur in the setting of high-energy trauma such as motor vehicle accidents or sports injuries [3]. The force applied by trauma can be applied either directly or indirectly onto the diaphysis of the radius and/or ulna. Direct injury frequently results from gunshot injuries or from blunt injury to the forearm. Indirect trauma on the other hand occurs either as bending or torsional forces. Bending forces can result in both bone forearm fractures that are located at similar segments along the diaphysis of the ulna and radius [2]. LCP can be used in forearm fractures in the conventional plating technique (compression method - principle of absolute stability) for simple transverse or oblique fracture with low soft tissue compromise or in the bridging technique (internal fixator method – principle of relative stability) for comminuted fractures if required ; or in the combination technique (compression and bridge technique) in special situation (e.g.segmental fracture with two different fracture pattern - one simple and one multi-fragmentary. It is unclear whether a bridging technique or a combination of compression and bridging is beneficial for simple transverse or oblique forearm fractures. Although the LCP represents the latest development in plate development, its usage in fractures with simple configuration and superiority is yet to be proved. Moreover, there are very few literatures published regarding the efficacy of LCP in weaker bone in adult’s patients.
Material and Methods
This prospective observational study was conducted at National Institute of Traumatology and Orthopaedic Rehabilitation from January to December 2018. Patients with diaphyseal both bone fracture of forearm aging 50 years and above were study population. Total 44 cases were included. Clinical, radiological and functional outcome were assessed and followed up for 24 to 30 (Average 25.27 weeks ± 1.39 weeks). Final functional outcome was done with Anderson criteria.
■ Protein preparation
After selecting a case according to inclusion and exclusion criteria, patients were evaluated pre-operatively. Pre-operative X-rays were taken. After preparing the patients, operation was done (detailed surgical procedure is given in Appendix V). During operation, stainless steel LCP was used. Long arm back slab was given post operatively. Injection Ceftriaxone was given per-operatively followed by oral Cefixime and Flucloxacillin for 14 days. Patients were discharged from hospital at 4th POD after removing drain. 1st follow up was given at 14th POD to check any signs of infection, pain status and distal neurovascular status. Cast was removed and active movement of elbow, shoulder and wrist was started. Stitch was removed on the same day. Next follow up were given at 6th week, 12th week and 24th week after operation. During these follow up session, range of motion was tested and X-Ray was done. VAS score for pain, quick DASH score and functional outcome according to Anderson criteria were measured during these follow ups. Assessment of any late complications was done. Improvement was noted. Data was processed and analyzed using computer software program SPSS version 25.0. The data present on categorical scale was expressed as frequency and corresponding percentage, while the quantitative data was presented as mean and Standard Deviation (SD)
Results
Total 44 patients involved in this study were followed up to one year. Maximum age incidence was found in 51-55 years of age. The mean age of the patients was 58.27 ± 5.68 years ranging from 51 years to 75 years. Out of 44 patients 35 (79.5%) were male and 9 (20.5%) were female. Male to female ratio was 3.86:1. Among 44 cases, 23 (52.3%) had left sided fracture and 21 (47.7%) had right sided fracture. In this study, motor vehicle accident accounted for 23 (52.3%) cases which was the most common cause of injury. Other causes were fall from height in 17 (38.6%) cases and physical assault in 4 (9.1%) in descending order. The mean radiological union time was 12.18 ± 1.53 weeks with 1 case of nonunion (TABLE 1).
| Sex | N (%) | Affected side of the cases | N (%) | Cause of Injury | N (%) |
|---|---|---|---|---|---|
| Male | 9 (20.5) | Right | 21 (47.7) | Motor vehicle accident | 23 (52.3) |
| Female | 35 (79.5) | Left | 23 (52.3) | Fall from height | 17 (38.6) |
| Physical assault | 04 (9.1) |
Among the cases, 17 (38.6%) fractures were 2R2A 2U2A type, 11 (25.0%) were 2R2A 2U2B type, 8 (18.1%) were 2R2B 2U2A type, 4(9.1%) were 2R2B 2U2B, 1 (2.3%) was 2R2C, 1 (2.3%) was 2R2B 2U2C, 1 (2.3%) was 2R2C 2U2C type and the remaining 1 (2.3%) was 2R2C 2U2C type (TABLE 2).
| Fracture Sub-type | Frequency | Percentage |
|---|---|---|
| 2R2A | 17 | 38.60% |
| 2U2A | ||
| 2R2A | 11 | 25.00% |
| 2U2B | ||
| 2R2A | 1 | 2.30% |
| 2U2C | ||
| 2R2B | 8 | 18.10% |
| 2U2A | ||
| 2R2B | 4 | 9.10% |
| 2U2B | ||
| 2R2B | 1 | 2.30% |
| 2U2C | ||
| 2R2C | 1 | 2.30% |
| 2U2B | ||
| 2R2C | 1 | 2.30% |
| 2U2C | ||
| Total | 44 | 100.00% |
Among 44 cases, 39 (88.6%) had no complications but the rest 5 (11.4%) had complications. Among the complications, tourniquet palsy occurred in 3 (6.8%) cases, deep SSI in 1 (2.3%) cases and superficial SSI in 1 (2.3%) cases (TABLE 3).
| Complication | Frequency | Percentage |
|---|---|---|
| No Complication | 39 | 88.60% |
| Tourniquet palsy | 3 | 6.80% |
| Deep SSI | 3 | 2.30% |
| Superficial SSI | 3 | 2.30% |
| Total | 3 | 100.00% |
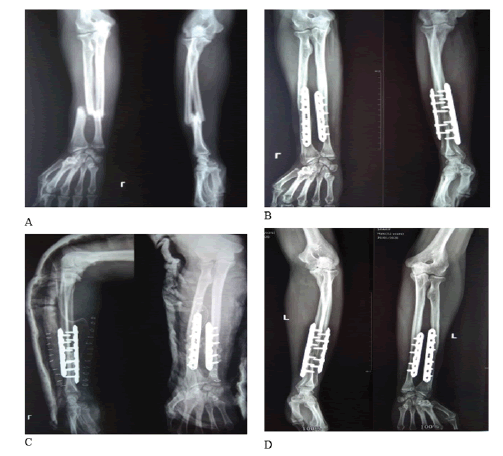
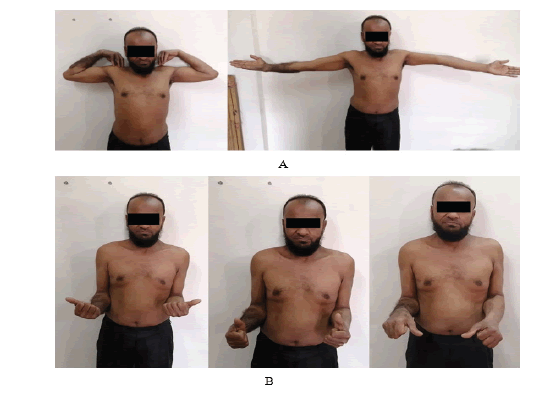
TABLE 4 shows that the patients according to duration of hospital stay showed the mean duration was 9.44 ± 2.31 days ranging from 6 days to 15 days. Most of the cases (n=39, 88.6%) were followed up for 24 weeks to 26 weeks. The remaining 5 (11.4%) were followed up for 27 weeks to 30 weeks. The average follow up period was 25.27 ± 1.39 weeks ranging from 24 weeks to 30 weeks. Among the 44 cases, 22 (50%) were excellent, 21 (47.7%) were good and the remaining 1 (2.3%) were poor. There was no fair outcome (FIGURE 1 to FIGURE 4).
| Hospital Stay (days) | N (%) | Follow up Period (In Weeks) | N (%) | Final outcome (Anderson criteria) | N (%) |
|---|---|---|---|---|---|
| 10-Jun | 32 (72.7) | 24-26 | 39 (88.6) | Excellent | 22 (50.0) |
| 15-Nov | 12 (27.3) | 27-30 | 05 (11.4) | Good | 21 (47.7) |
| Mean ± SD | 9.44 ± 2.31 | Mean ± SD | 25.27 ± 1.39 | Poor | 01 (2.3) |
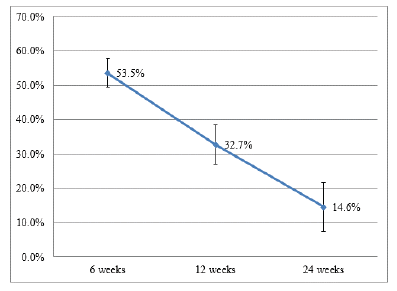
Six weeks after surgery, the mean Quick DASH score of the cases were 53.5% ± 4.13%. At 12 weeks, it has decreased to 32.7% ± 5.73%. Furthermore, at last follow up, it has significantly decreased to 14.6% ± 7.14% (p value=2 × 10-31).
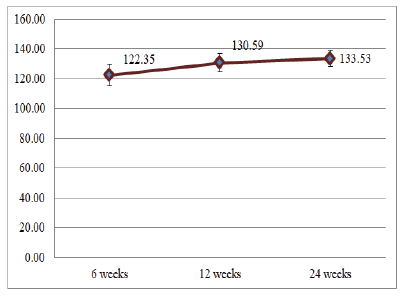
The mean arc of motion (Flexion-Extension) of elbow at first follow up was 122.35° ± 7.09° . The mean arc of motion at 2nd follow up was 130.59° ± 6.25° . Finally, at last follow up it has significantly improved to 133.53° ± 5.44° . From 1st follow up to last follow up, arc of motion has significantly improved (p value=8×10-17).
Discussion
Locking Compression Plates (LCPs) combine the properties of both locking plates and DCPs. With their combined hole, an unlocked compression screw and a locking screw can be used. Locking compression plates have been shown to provide a stronger fixation compared with DCPs in biomechanical studies. In addition, LCPs can be placed using a bridging plate technique, allowing biological fixation for the treatment of comminuted fractures. These advantages of the LCP have been considered to accelerate fracture healing and reduce the problems of delayed union and non-union [4,5]. In this study the mean age of the patients was 58.27 years ± 5.68 years ranging from 51 years to 75 years. Maximum age incidence was found in 51 years-55 years of age. (n=18, 40.9%). Among remaining study patients, 13 cases (29.5%) belonged to 56 to 60 age group, 9 (20.5%) in 61 to 65 age group, 3 (6.8%) in 66 to 70 age group and the remaining 1 (2.3%) in 71 to 75 age group. In other several studies who tried to find out the efficacy of LCP, the mean age ranged from 30 years to 38 years [6-8]. Out of 44 patients 35 (79.5%) were male and 9 (20.5%) were female. In the series of Iacobellis & Biz, male were 93% and female were 7% with a male to female ratio of 13:1 [9]. The present series showed a higher percentage of female than the series of Iacobellis & Biz [9]. This may be due to more osteoporotic fractures in female in the present series. Among 44 cases, 23 (52.3%) had left sided fracture and 21 (47.7%) had right sided fracture. In the study of Ravi et al, (2014) the left side was involved in 19 (45%) patients & 21 (55%) had right side involvement [8]. The results are quite similar to the present study. In this study, motor vehicle accident accounted for 23 (52.3%) cases which was the most common cause of injury. Other causes were fall from height in 17 (38.6%) cases and physical assault in 4 (9.1%) in descending order. In the series of Henle et al, (2011) motor vehicle accidents were identified as the predominant cause of injury (n = 26, 59.1%) [10]. Among the cases, 17 (38.6%) fractures were 2R2A 2U2A type, 11 (25.0%) were 2R2A 2U2B type, 8 (18.1%) were 2R2B 2U2A type, 4(9.1%) were 2R2B 2U2B, 1 (2.3%) was 2R2C, 1 (2.3%) was 2R2B 2U2C, 1 (2.3%) was 2R2C 2U2C type and the remaining 1 (2.3%) was 2R2C 2U2C type. Previous studies working with diaphyseal fractures of both bones did not use the latest AO classification system. For example, in the series of Saikia et al, (2006), 21 (58.33%) were type A, 13 (36.11%) were type B and the remaining 2 (5.56%) were type C fractures [6]. Out of 44 cases, in 19 (43.2%) cases, operation was done between 11 days to 15 days after injury. In 21 (47.7%) cases, duration was 16 days to 20 days and in remaining 4 (9.1%) cases it was 21 days-25 days. The mean duration of injury to operation was 16.29 days ± 3.35 days, ranging from 11 days to 25 days. In cases, where final outcome were excellent, the mean duration of injury to operation was 14.18 days ± 1.59 days. Whereas, in cases with either good or poor outcome, the mean duration of injury to operation was 18.41 days ± 3.34 days. In the study of Azboy et al, (2013), average time from injury to surgery was 3 days (range, 1-8 days) [5]. There was significant delay of operation in the present series. Distribution of patients according to duration of hospital stay showed the mean duration was 9.44 days ± 2.31 days ranging from 6 days to 15 days. Among 44 cases, 39 (88.6%) had no complications but the rest 5 (11.4%) had complications. Among the complications, tourniquet palsy occurred in 3 (6.8%) cases, deep SSI in 1 (2.3%) cases and superficial SSI in 1 (2.3%) cases. In the series of Saikia et al, (2011), where they found a patient developed transient radial nerve palsy postoperatively, which improved with conservative management by the 6th postoperative week [6]. Out of 44 cases, 43 (97.7%) was united but only 1 (2.3%) case neither unite nor found any sign of union up to 29 weeks of follow up. This was due to deep infection which has led to implant removal followed by refashioning of the fracture site and internal fixation by LCP with autogenous cancellous bone graft. Deep infection is a grave consequence which ultimately leads to nonunion as shown in several studies. Ravi et al, (2017) reported nonunion in 2 of their cases and all due to deep infection [7]. Among the 44 cases, 22 (50%) were excellent, 21 (47.7%) were good and the remaining 1 (2.3%) were poor. There was no fair outcome. The poor outcome was due to nonunion of that case. Saikia et al, (2011), found excellent in 88% cases and good in 12% of their cases [6]. As no nonunion occurred in their cases, so there was no poor outcome. Moreover their follow up period was 22 months, less mean age of the study cases and early surgery of the cases resulted their more excellent outcome. Likewise, in the series of Iacobellis & Biz, they found 91.5% of their cases were united [9].
Conclusions
In concluded, use of LCPs represents an effective treatment in terms of union rate, pain and functional outcomes. The major mechanism of these fractures is Motor vehicle accident. Most common fractures in leftside. In this study, the surgical outcomes were excellent in 50% of cases, 21 (47.7%) were good and the remaining 1 (2.3%) was poor. Internal plating gives good functional results in the treatment of forearm diaphyseal fractures, as long as the surgical technique is perfect.
References
- Leung F, Chow SP. Locking compression plate in the treatment of forearm fractures: a prospective study. J orthop surg. 14(3), 291-294 (2006).
[Google Scholar] [Crossref]
- Streubel PN, Pesantez RF. Diaphyseal fractures of the radius and ulna. InRockwood, Green, and Wilkins Fractures in Adults and Children: Eighth Edition. Wolters Kluwer Health Adis. (2014).
[Google Scholar][Crossref]
- Bot, A. G., Doomberg, J. N., Lindenhovius, A. L. & Ring, D.. Long-term outcomes of fractures of both bones of the forearm. J Bone Jt Surg. 93(6), 527-532 (2011). [Google Scholar]
[Crossref]
- AO Foundation, 2018. Fracture and Dislocation Classification Compendium 2018. J Orthop Trauma. 32, 49-53. [Google Scholar]
[Crossref]
- Azboy Ä°, Demirtas A, Uçar BY, Bulut M, Alemdar. Effectiveness of locking versus dynamic compression plates for diaphyseal forearm fractures. Orthopedics. 36(7), 917-922 (2013 ).
- Saikia KC, Bhuiyan SK, Bhattacharya TD, Ahmed F. Internal fixation of fractures of both bones forearm: Comparison of locked compression and limited contact dynamic compression plate. Indian j orthop. 45(5), 417 (2011).
- Gill SP, Mittal A, Raj M, Singh P, Kumar S. Stabilisation of diaphyseal fractures of both bones forearm with limited contact dynamic compression or locked compression plate: comparison of clinical outcomes. Int J Res Orthop. 3(3), 623-631 (2017).
- Ravi KB, Raghavendra TS, Balasubramanian S. Forearm Bone fractures: Dynamic Compression Platting Vs Locking compression plating–Randomised control study. Indian J Basic Appl Med. Res. 3(3), 226-232 (2014).
[Google Scholar] [Crossref]
- Iacobellis C, Biz C. Plating in diaphyseal fractures of the forearm. Acta Biomed. 84(3), 202-211(2014).
[Google Scholar] [Crossref]
- Henle P, Ortlieb K, Kuminack K, Mueller CA, Suedkamp NP. Problems of bridging plate fixation for the treatment of forearm shaft fractures with the locking compression plate. Arch orthop trauma surg. 131, 85-91 (2011).