Research Article - (2022) Volume 5, Issue 3
Photobiomodulation and its Application in Dentistry
Shaymaa Hussein Rafat Kotb*Received: Oct 27, 2022, Manuscript No. AMDHS-22-78364; Editor assigned: Oct 28, 2022, Pre QC No. AMDHS-22-78364 (PQ); Reviewed: Oct 30, 2022, QC No. AMDHS-22-78364 (Q); Revised: Oct 31, 2022, Manuscript No. AMDHS-22-78364 (R); Published: Nov 10, 2022, DOI: 10.5530/amdhs.2022.3.8
Abstract
Introduction: Photobiomodulation is a promising field in modern minimally invasive dentistry approach which serves as a non-cutting method of using the red to near infrared light on body tissues. PBM consider an excellent alternative or adjunctive to traditional treatment modality. It is a simple and fast to perform, well accepted and tolerated by the patients, that aid in pain relief and reduces inflammation, parallel to the enhanced healing and tissue repair processes. PBM can induce cell proliferation and enhance stem cell differentiation. This impact has direct effects on many stimulatory and protective genes. So this application with these properties was used as adjunctive therapy to the conventional treatment of various diseases and conditions related to soft and hard tooth structure and surrounding tissues.
Aim: The purpose of this study is to thorough the light on the applications of PBM therapy in dentistry by understand mechanism of action, with a special focus on stem cells and mechanisms of repair.
Methods: A systematic literature review depends on collecting data from an evidence based studies. Searches were made of fifteen electronic databases: the Cochrane Oral Health Group’s Trials Register, The Cochrane Central Register of Controlled Trials (CENTRAL), EMBASE, PsycINFO, Scopus and Web of science, MEDLINE (PubMed).
Summary: PBM applications is very promising adjunctive or alternative approach in periodontal, Peri-implant inflammation therapy, orthodontic treatment, temporomandibular joint problems, and with oral medicine lesions, surgical exposure of impacted teeth, pediatric dentistry, crown cementation, dentin hypersensitivity and in gingivectomy, gingivoplasty and frenectomy. LLLT is an easy, simple, shorter chair time, mostly technique accepted by patients and moreover reduce pain intensity, stimulate healing capacity, better coagulation and no need for suturing so gain more patients acceptance.
Conclusion: Photobiomodulation is recommended as an alternative for failed standard therapy or as an adjunct modality to treatments. It is a safe and potentially effective on its own thus facilitating easy use. It is a helping device to complete conventional therapy. With superior advantages of easy and faster application, better coagulation, no need for suturing, less swelling and pain and better deepithelialization. However, there is some limitations include cost of the device and it is very difficult to have all the different lasers indicated for different procedures in a private practice.
Keywords
Photobiomodulation, Laser therapy, Diode laser, LLLT, Minimal invasive dentistry, Cosmotic dentistry
Introduction
The importance of light in our biological systems and processes can be seen clearly in our sleep–wake cycles, circadian rhythms, and in the absorption of vitamins. From this point our research is to thourogh the light on using the high-powered light (at specific wavelengths) in biology, creating a new perspective for its application in healing, protect the cells from dying and tissue engineering. LASER means a Light Amplification and Stimulated Emission Radiation. This is a device which produces light which is inphase (have the same frequency) is called coherent light. Lasers can be categorized as hard tissue lasers and soft tissue lasers, depending upon the type of laser-tissue interaction. Laser tissue interaction is dependent upon wavelength, tissue type, power (incident energy), and time. Wheresoever’s, the effect is ablative (essentially photothermic), direct and primary, such lasers are termed ‘hard like Carbon dioxide, NdYAG, and Er:YAG. They can be used for both hard and soft tissue application but they have limitations as they are expensive and cause thermal injury to the tooth pulp. Alternatively, where tissue effects are non-direct and through secondary (essential biostimulatory), intermediate action, such lasers are termed ‘soft’ or cold laser. This group also can be termed Low-Level Lasers Therapy (LLLT), Low Power Laser Therapy (LPLT), cold laser, biostimulation laser, bioregulation laser, photobiomodulation, photomedicine, medical laser, therapeutic laser, healing laser, non-thermal laser, low-intensity laser, lowreactive laser [1].
Photobiomodulation, is the application of specific wavelengths of light with a narrow spectral bandwidth light from red to near-infrared light with a power density of 1 mW/cm2 to 5000 mW/cm2 to modulate cell metabolism, signal transduction, and secretion in the body tissues (∼λ=600-1000) by reduce inflamation, accelerate healing, and increases cell viability by stimulating the mitochondrial and cell membrane photoreceptors synthesis of ATP. This process can be used in promoting the proliferation of osteoblasts so stimulate bone healing. That photons can stimulate a chemical change in neurones, that light energy can be converted to metabolic energy with a subsequent influence on the function and survival of the neurones. Photobiomodulation is not a targeted treatment; it can potentially adjunctive therapy to any neurone in distress [2].
Photobiomodulation (PBM), is a non-invasive, non-cutting treatment modality by using Low-Level Laser Light Therapy (LLLT), to produce low intensity energy light to provide pain relief by producing analgesic effect by inhibiting nociceptive signals ,moreover decrease inflammation and subsequent healing. In dentistry, it is used as an adjunct that supplements many hard and soft tissue procedures. So it seems to be an alternative approach of choice to address the need for immune regulation which especially used in Covid-19 crisis to immune regulate the cytokine storm in the bloodstream by T cells and macrophages, of which IL1-b, IL-2, IL- 8, IL-10, IL-6, IL-12, IFN-g, and TNF [3 4].
The cornerstone area of interest concerning PBM is its effect on susceptible stem cells, progenitor cells, and its potential in enhancing differentiation, and so improves the healing ability of tissues. The proliferation of stem cell improved by photobiomodulation, such as gingival fibroblasts, dental pulp stem cells extracted from permanent teeth, exfoliated deciduous teeth, in addition to mesenchymal stem cells derived from bone marrow or adipose tissue. It can increase collagen production, the mitotic activity of epithelial cells and fibroblast [5].
The application of LLLT also stimulates various cells lymphocytes and mast cell which will produce anti-inflammatory actions causing changes in the capillary hydrostatic pressure which results in oedema absorption and elimination of intermediary metabolites. Even it can increase collagen production, the mitotic activity of epithelial cells and fibroblast. Moreover, it can produce an analgesic effect by inhibiting nociceptive signals [6].
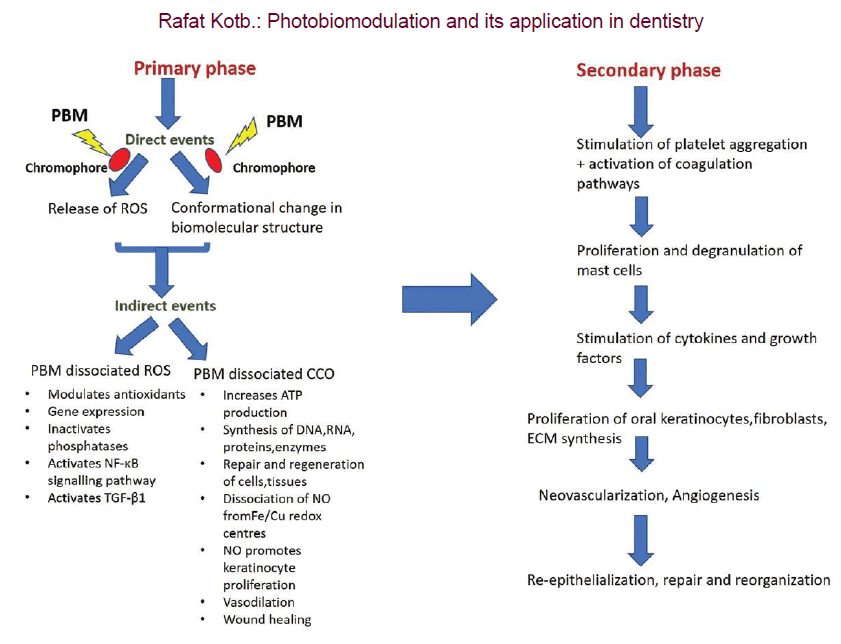
Impact of PBM on cells aid in improved healing. For example, one theory states that PBM reacts with target cells photo-chemically. Mitochondria contain chromophores which absorb photons from PBM that result in encourages the activity of production of molecules such as Nitric Oxide (NO), ATP, calcium ions, Reactive Oxygen Species (ROS), and other signaling molecules. Regulation of ROS levels is important, as it affects several signaling pathways responsible for the development and proliferation of stem cell. Bone healing is improved by laser therapies accelerating stem cell differentiation into osteoblasts and bone cells, and also through increasing calcium transport during the formation of bones [7, 8].
The mechanism of action for PBM on cells is photon radiation posits either directly or indirectly targeting DNA and the genome pool. Free radicals (including ROS) are produced on the impact of indirect, low laser radiation. High levels of ROS are cytotoxic, leading to multiple signaling cascades being interrupted. However, in low levels, ROS can be beneficial to red blood cells. ROS can generate normal metabolism in the production of ATP synthesis and regulate proteins that are affected by redox reactions and involved in proliferation and differentiation. Cyclooxygenase (COX) enzymes are involved in the normal run of the membrane potential of the mitochondria and collect ROS to ensure this. These enzymes stop the production of unnecessary ROS when the mitochondrial membrane potential has decreased, due to various factors caused by toxic environments, such as oxidative stress, damaged neurons, or the suppression of electron transport. While ROS production is stopped, COX will act to restore the mitochondrial potential back to normal levels. Regulation of ROS levels is important, as it affects several signaling pathways responsible for the development and proliferation of stem cells [9].
PBM enhancing bone regeneration which enhances both differentiation and proliferation of mesenchymal stem cells into ostogenic bone cells so encourage the body’s natural repair/healing capability. Another technique of pulse repetitive laser radiation induces porous activity by introducing repetitive heat in the tissue thus stimulating angiogenesis by newly made blood vessels. The process of forming pores starts in area of heat that reaches cold areas, and this causes local strains and disruption of homeostasis. So, laser therapy approach can aid the process of tissue repair and regeneration is by increasing bone grafts porosity. It is the application of laser light energy to living tissues to generate biosimulation effects without causing an excessive rise in temperature [10, 11].
Lasers with different characteristics have been employed in different branches of dentistry. Depending on the composition of semi-conductors, a wave with different frequency (length) can be generated. Diode lasers consists of wavelengths of 445 nm to 980 nm which stimulate wound healing after surgery, Some of the most popular lasers in implant surgery for cutting soft tissues are lasers with waves in the range of 808 nm-980 nm [12, 13].
Dental Laser, like CO2 and diode lasers used for the decontamination of the implant surface. Nd:YAG and Er:YAG lasers at low-intensity have bactericidal effects. Herefore, when used to decontaminate and regenerate peri-implant bone defects, dental lasers may be a viable option for positively affecting RBL changes during peri-implantitis treatment. LLLT may enhance bone gain in peri-implantitis defects, reduce BOP and PDs [14].
Laser and Light-Emitting Diodes (LEDs) are widely used in almost every field of clinical dentistry, and for the therapy of numerous diseases like candidiasis treatment, burning mouth syndrome and periodontitis and in the prevention of chemotherapy-induced oral mucositis. PBM used in orthodontic treatment to alivate pain after orthodontic appliance placement and in orthodontic ceramic brackets cementation. It also improves osseointegration, collagen deposition, and achieves faster bone-remodeling, In surgical-assisted therapy, such as implant and mini-implant placement, it was shown to assist implant stability and improves osseointegration, collagen deposition, and achieves faster bone-remodeling and reduce healing time along with swelling, so improvement of postoperative comfort and in and in temporomandibular joint problems. LLLT can be applied directly to the superficial mucosa before the injection, which will produce a good anesthetic effect. All this applications changing the dental healthcare approaches and patient’s quality of life [15-18].
There is a great interest on application of Laser therapy on oral medicine conditions, like recurrent aphthous ulcer for immediate relief pain and improve wound healing. PBM can also used in recurrent herpes infections which resistant to treatment. The primary benefit is that it is a non-surgical technique, which will reduce the incidence of oedema and inflammations. The cellular targets for PBM include the inhibition of cyclooxygenase resulting in the reduced production of prostaglandins, which act as key mediators of the acute inflammatory response. Consequent to the analgesic and anti-inflammatory actions of PBM, it has been proposed as a tool that may permit a locally directed alternative to systemic drugs without the risks of allergy, toxicity, impaired healing and other important medical issues such as addiction [19-21].
Modern paediatric dentistry use (LLLT) in Caries Detection and Diagnosis: By using diagnodent (Kavo, Biberach, Germany, a portable laser diode based device, in Pulpotomy). The main advantages of laser-assisted pulpotomies were: less chair side time and painless procedure thus increasing paediatric patient’s co-operation. The Diode laser is the most frequently used due to its reliability, versatility and convenience, together with its handiness and simple set-up. Lasers apply in Apexogenesis in children so reinforces the overall sterilizing procedure, and laser coagulation produces a thin necrotic layer over the vital remaining pulp. The advantage of this application, vital pulp responds in the formation of a dentin bridge. Another modern application of LLLT in Frenectomy, which carried out with diode laser at a wavelength of 800 nm and power of 2 W in non-contact mode proved that the laser can be considered as a simple and safe alternative for children while reducing the amount of local anaesthetics, the bleeding and the chances of infection, swelling and discomfort [22-25].
LLLT can be used in treatment oral mucosal lesion like lichen planus, which considered a type of disease which has an unknown cause. The T-lymphocytes are the ones that are responsible for the pathogenesis, notreatment is needed except for relief burning sensation and to preventfurther malignant transformation. In addition, there are two types of theeffects that a low-level laser produces: primary and secondary. Primarily, itcauses vasodilation, lymphatic drainage, cellular activity and metabolism,enhancement of the flow of blood, activation of fibroblast and neutrophils, and stimulation of pain threshold. The secondary effect is the aggregationof prostaglandin, immunoglobulin and lymphocytes, and beta-endorphinin the tissue encephalin. Therefore, this will reduce infectionand inflammation, pain, soreness, and immuneresponse [26].
Oral leukoplakia has also shown regression with laser therapy. CO2 lasers are very beneficial in treating oral leukoplakia. It causes minimal swelling and pain. Photodynamic therapy with 5-aminolevulinic acid and apulse dye laser is used to maintain the regression of the leukoplakia. Although it is less invasive and painful and it shows better aesthetics, there has been a reoccurrence of the dysplastic oral leukoplakia after oral surgery in the instances of smoking directly after the surgery. So, changes in oral habits have a great influence on the outcome of the laser surgery [27].
Oral mucositis which is considered as the most painful oral lesion requires narcotic analgesic and can reduce the quality of life. Factors that influence the growth of the oral mucositis are chemotherapeutic regimen, the type of malignancy, patients’ age, neutrophil counts and the use of oral care measure. There are many side effects for the oncologic therapy such as ulcerations, alopecia, thrombocytopenia, neutropenia, and oropharyngeal mucositis. The condition is worsened if accompanied by poor oral hygiene, pre-existing intraoral lesions, deficient immune status, and high-level proinflammatory cytokines. The most involved tissues are the non-keratinized tissues, the lateral borders of the tongue, and the floor of the mouth, and many therapeutic and preventive measures such as analgesics, cryotherapy, antibiotics, anti-inflammatory agents’ growth factors and biological mucosal protectants should be prescribed. The application of LLLT has shown a significant reduction in the pain associated with oral mucositis as well as quicker healing of the oral lesions [28].
Another LLLT application with Fordyce granule excision using a combination of the low-intensity and high-intensity lasers has produced increased aesthetics results and quicker healing with reduced postoperative pain and inflammation [29].
In recent years, dental manufacturers have introduced a new generation of zirconia ceramics that are suitable for tooth reconstruction in the esthetic zone. High-Translucent Monolithic Zirconia (HTZ) has gained much interest from patients with esthetic demands because of its superior optical properties. HTZ materials possess significantly lower flexural strength (550 MPa to 800 MPa instead of 900 MPa to 1400 MPa), and even poorer adhesive behavior with resin based cements as compared to conventional zirconia. Laser surface treatment of HTZ ceramics is a promising alternative method to enhance the mechanical retention of resin cement as it is related to effective bond strengthening, without causing any surface contamination of zirconia specimens [30].
Laser therapy could improve Self-Adhering Flowable Composite (SAC) dentinal bond strength after thermocycling and significantly increased Shear Bond Strength (SBS) in comparison to non-irradiated dentin so improving its longevity [31].
Diode laser 980 nm is in the near infrared position of the electromagnetic spectrum. A part of this energy is absorbed by the dentinal components provoking melting of the dentin structure. The absorption coefficients of diode lasers are low in dentin which propagate generation of heat on pulp and so irreversible pulpitis so the application of graphite paste enhances the absorption of the beam on the dentin surface since prevent undesirable effect on pulp. The graphite will also provoke an important increase of temperature localized at the dentinal surface to close the dentinal tubules and so aid in treatment dentinal hypersensitivity [32].
Currently, there are a lot of laser wavelengths that are used in dentistry, specifically oral surgery, including CO2, Argon, Nd YAG, KTP that are applied in various specialties in dentistry including the caries diagnosis and removal, light curing of the composite, control of bleeding in vascular lesions. Furthermore, they have been used in the temporomandibular joint surgery, the activation of tooth bleaching solutions, and the soft tissue procedures, for example, gingivectomy, gingivoplasty, excision of tumours, excision of biopsies, and second stage recovery of implants [6].
Results
There is a positive clinical outcome of using PBM modality in modern dentistry approach. Laser dentistry has been a benchmark in dentistry and is truly the future of this field. PBM or LLLT show significance value as adunctive or alternative to failed or resistant conventional modality treatment. LLLT is an easy ,simple ,shorter chair time, mostly technique accepted by patients and moreover reduce pain intensity, stimulate healing capacity, better coagulation and no need for suturing so gain more patients acceptance moreover reduce clinician fatigue and stress (TABLE 1-3).
| Parameter | Value/Description |
|---|---|
| Light type | Low power laser or LED |
| Radiation power range | 10 mW-500 mW |
| Mode of laser operation | Continuous, modulated, and pulsed |
| Power density (irradiance) | 5 W/cm2 |
| Beam power | 1 W |
| Spectrum | Red to infrared region |
| Wavelength | 760 nm-850 nm |
| Light density | 5 mW/cm2 at 5 cm deep |
| Surface density | 5 W/cm2 |
| Application time | 30 Seconds-60 Seconds |
| Gas lasers | Liquids | Solid | Semiconductor | Excimers |
|---|---|---|---|---|
| Argon | Dyes | NdYAG | Hybrid silicon laser | Argonfluoride |
| Carbon-dioxide | Er:YAG | Kryptofluoride | ||
| Diode | Xenonfluoride |
| Culture Group | Energy Density (J/cm2) | Enhanced Proliferation and Differentiation Induced Cell Type |
|---|---|---|
| 1 | 2 | Osteoblast |
| 2 | 3 | Neural |
| 3 | 4 | Osteoblast |
| 4 | 6 | Neural |
Discussion
The therapy PBM or low laser intensity is considered a new alternative or adjunctive to conventional treatment modality. Photobiomodulation improves neuronal and mitochondrial activity function and so stimulating a range of protective pathways, improvements in clinical signs and/ or symptoms in a range of disorders (FIGURE 1). Laser therapy have many applications, like regenerative medicine, cosmotic dentistry such as depigmentation of hyperpimented gingiva, and root canal disinfections and pain reduction following orthodontic elastomeric separation. Lasers are certainly the future for dentistry as it makes it very easy to use. It is very helpful when reaching areas that were hard to treat with traditional treatments. There is low risk of infections in and around the treatment area. Laser dentistry has been a benchmark in dentistry and is truly the future of this field. Diode laser is safe and well indicated for soft oral tissue surgeries in regions near the dental structures for cutting, vaporization, curettage, blood coagulation and haemostasis in the oral region. The chromophore of diode lasers is pigmented (or coloured) tissues, specifically melanin, haemoglobin and oxyhemoglobin. The diode is efficient for treating the patient’s soft tissues because the gingival tissues have a concentration of these chromophores; as a result, a diode photon has a high affinity for gingival tissues. Its use in contact mode provides tactile feedback during surgical procedure. The main advantages of the laser therapy over scalpel surgical procedures on oral tissues are greater precision, bloodless surgical procedures, sterilization of the surgical area, minimal swelling and scarring, no suturing, and less or no postsurgical pain. Clinicians should be careful to prevent inadvertent irradiation to these tissues, especially to the eyes. Protective eyewear specific for the wavelength of the laser in use must be worn by the patient, operator, and assistant. Laser beams can be reflected by shiny surfaces of metal dental instruments, causing irradiation to other tissues, which should be avoided by using wet gauze packs over the area surrounding the target. There are also some Potential risks like, Excessive tissue destruction by direct ablation and thermal side effects and Thermal injury to the root surface, gingival tissue, pulp, and bone tissue. LLLT has absolute contraindications in patients with coagulation disorders because it has a direct effect on blood flow and in cases of malignancies because it stimulates cell growth. The FDA classifies low-level lasers into low-risk devices because it is not harmful. The therapeutic laser is less than 500 mW. There is still some Limitation: PBM can be inconvenient for patients who have poor access to a medical facility, or who have limited availability in their schedule to commit to regular clinic visits. The cost of the device, and there is variability in the devices and treatment parameters used so lack of standard protocol. Efforts should be directed toward investigating the precise dosimetry required for therapeutic laser effects, in order to achieve standardization of treatment protocols. Improvements in the design of LLLT equipment are necessary to enable the various techniques to be accomplished within an adequate time frame and without breaching cross-infection.
Conclusions
It is important to highlight the role of using of photobiomodulation therapy in Advanced Modern Dentistry. Photobiomodulation or LLLT is a safe and potentially effective modality for the management. PBM applications is very promising adjunctive or alternative approach in periodontal, peri-implant inflammation therapy, orthodontic treatment, temporomandibular joint problems, and with oral medicine lesions. The idea of the photobiomodulator effect of low-level laser can help in reduce use of conventional pharmacological treatment, so that the dose of corticosteroids can be reduced, and thus also attenuates the side effects of medications treatment. LLLT is an easy, simple, shorter chair time, mostly technique accepted by patients and moreover reduce pain intensity, stimulate healing capacity, better coagulation and no need for suturing so gain more patients acceptance.
Recommendation
The clinician should be well educated in dental lasers and abide by the laser guidelines and protocols of the manufacturer, to ensure safe use of the laser in patient treatment.
Funding
None
Competing Interests
The authors declare that they have no competing interests.
Ethical Considerations
Not applicable
References
- Anders JJ, Lanzafame RJ, Arany PR.Low-level light/laser therapy versus photobiomodulation therapy. Photomed Laser Surg. 33(4), 183-184 (2015).
- Khadra M, Lyngstadaas SP, Haanæs HR, Mustafa K. Effect of laser therapy on attachment, proliferation and differentiation of human osteoblast-like cells cultured on titanium implant material. Biomaterials. 26(17), 3503-3509 (2005).
- De Freitas LF, Hamblin MR. Proposed mechanisms of photobiomodulation or low-level light therapy. IEEE J Sel Top Quantum Electron. 22(3), 348-364 (2016).
- Li X, Geng M, Peng Y, Meng L, Lu S. Molecular Immune Pathogenesis and Diagnosis of COVID-19. J Pharm Anal. 10(2), 102-108 (2020).
- Fernandes AP, Junqueira MDA, Marques NCT et al. Effects of low-level laser therapy on stem cells from human exfoliated deciduous teeth. J Appl Oral Sci. 24, 332-337 (2016).
- Convissar RA. Principles and Practice of Laser Dentistry-E-Book. Elsevier Health Sci. 2015.
[Google Scholar] [Crossref]
- Migliario M, Pittarella P, Fanuli M, Rizzi M, Renò F. Laser-induced osteoblast proliferation is mediated by ROS production. Lasers Med Sci. 29(4), 1463-1467 (2014).
- Son JH, Park BS, Kim IR et al. A novel combination treatment to stimulate bone healing and regeneration under hypoxic conditions: Photobiomodulation and melatonin. Lasers Med Sci. 32(3), 533-541 (2017).
- Dos Santos SA, Serra AJ, Stancker TG et al. Effects of Photobiomodulation Therapy on Oxidative Stress in Muscle Injury Animal Models: A Systematic Review. Oxid Med Cell Longev. (2017).
- De Witte TM, Fratila-Apachitei LE, Zadpoor AA, Peppas NA. Bone tissue engineering via growth factor delivery: From scaffolds to complex matrices. Regen Biomater. 5(4), 197-211 (2018).
- Baum OI, Zheltov GI, Omelchenko AI et al. Thermomechanical effect of pulse-periodic laser radiation on cartilaginous and eye tissues. Laser Phys. 23(8), 085602 (2013).
- Matys J, Flieger R, Dominiak M. Effect of diode lasers with wavelength of 445 and 980 nm on a temperature rise when uncovering implants for second stage surgery: An ex-vivo study in pigs. Adv Clin Exp Med. 26(4), 687-693 (2017).
[Google Scholar] [Crossref]
- Gomes FV, Mayer L, Massotti FP et al. Low-level laser therapy improves peri-implant bone formation: Resonance frequency, electron microscopy, and stereology findings in a rabbit model. Int J Oral Maxillofac Surg. 44(2), 245-251 (2015).
- Mizutani K, Aoki A, Coluzzi D et al. Lasers in Minimally Invasive Periodontal and Peri-Implant Therapy. Periodontol 2000. 71(1), 185-212 (2016).
- Grzech-LeÅ?niak K, Sculean A, GaÅ¡pirc B. Laser reduction of specific microorganisms in the periodontal pocket using Er:YAG and Nd:YAG lasers: A randomized controlled clinical study. Lasers Med Sci. 33(7), 1461-1470 (2018).
- Lalla RV, Bowen J, Barasch et al. MASCC/ISOO clinical practice guidelines for the management of mucositis secondary to cancer therapy. Cancer. 120(10), 1453-1461 (2014).
- Artés-Ribas M, Arnabat-Dominguez J, Puigdollers A. Analgesic effect of a low-level laser therapy (830 nm) in early orthodontic treatment. Lasers Med Sci. 28(1), 335-341 (2013).
- Aras MH, GüngörmüÅ? M. The Effect of Low-Level Laser Therapy on Trismus and Facial Swelling Following Surgical Extraction of a Lower Third Molar. Photomed Laser Surg. 27(1), 21-24 (2009).
- Tezel A, Kara C, Balkaya V, Orbak R. An Evaluation of Different Treatments for Recurrent Aphthous Stomatitis and Patient Perceptions: Nd: YAG Laser versus Medication. Photomed Laser Surg. 27(1), 101-106 (2009).
- Stona P, Da Silva Viana E, dos Santos Pires L, Weber JB, Kramer PF. Recurrent Labial Herpes Simplex in Pediatric Dentistry: Low-level Laser Therapy as a Treatment Option. Int J Clin Pediatr Dent. 7(2), 140-143 (2014).
- Ross G. Photobiomodulation Therapy: A Possible Answer to the Opioid Crisis. Photobiomodulation Photomed Laser Surg. 37(11), 667-668 (2019).
- Franscesut P, Lussi A. Correlation between fissure discolouration, diagnodent measurements and caries depth: An in vitro study. Pediatr Dent. 25(6), 559-564. (2003)
[Google Scholar] [Crossref]
- Maturo P, Perugia C, Docimo R. Versatility of an 810 nm diode laser in paediatric dentistry. Int J Clin Dent. 6(2), 161-72 (2013).
[Google Scholar] [Crossref]
- Mathur VP, Dhillon JK, Kalra G. A new approach to facilitate apexogenesis using soft tissue diode laser. Contemp Clin Dent. 5(1), 106-109 (2014).
- Boj J, Galofre N, Espana A, Espasa E. Pain perception in paediatric patients undergoing laser treatments. J Oral Laser Appl. 5(2), 85-89 (2005).
[Google Scholar] [Crossref]
- Mahdavi O, Boostani N, Jajaram H, Falaki F, Tabesh A. Use of low level laser therapy of oral lichen planus. J Dent. 14(4), 201-204 (2013).
[Google Scholar] [Crossref]
- Montebugnoli L, Frini F, Gissi DB et al. Histological and immunohistochemicalevaluation of new epithelium after removal of oralleukoplakia with Nd: YAG laser treatment. Laser Med Sci. 27(1), 205-210 (2012).
- Cauwels RG, Martens LC. Low level laser therapy in oralmucositis: A pilot study. Eur Arch Paediatr Dent. 12(2), 118-123 (2011).
- Baeder FM, Pelino JE, De Almeida ER, Duarte DA, Santos MT. High-power diode laser use on Fordyce granuleexcision: A case report. J Cosmet Dermatol. 9(4), 321-324 (2010).
- Blatz MB, Vonderheide M, Conejo J. The Effect of Resin Bonding on Long-Term Success of High-Strength Ceramics. J Dent Res. 97(2), 132-139 (2018).
- Lin S, Pan D, Lin Q et al. Evaluation of phase, microstructure and composition of human dentine after Er, Cr: YSGG laser irradiation. J Nanosci Nanotechnol. 11(3), 2421-2426 (2011).
- Umana M, Heysselaer D, Tielemans M et al. Dentinal Tubules Sealing by Means of Diode Lasers (810 and 980 nm): A Preliminary In Vitro Study. Photomed Laser Surg. 31(7), 307-314 (2013).