Research Article - (2022) Volume 5, Issue 3
Techniques For Fertility Preservation In Patients With Breast Cancer - A Current Approach
Mariam Faruqui Shati1*, Bipasha Ahmed2, Md. Khorshed Alam3, Ashikur Rahaman4, Angel Tincy Abraham5 and Swati Sharma62Consultant, Clinical Embryology, Labaid Specialized Hospital, Dhaka, Bangladesh
3Prof. Head of Department (Radiation Oncology), Gonoshasthaya Samaj Vittik Medical College, Savar, Dh, Bangladesh
4Consultant, Department of Clinical Oncology, Enam Medical College Hospital, Savar, Dhaka,, Bangladesh
5Senior Embryologist, International Fertility Center, Delhi, India
6Fellow, International Fertility Center, Delhi, India
Received: Nov 03, 2022, Manuscript No. AMDHS-22-78364; Editor assigned: Nov 05, 2022, Pre QC No. AMDHS-22-78364 (PQ); Reviewed: Nov 07, 2022, QC No. AMDHS-22-78364 (Q); Revised: Nov 08, 2022, Manuscript No. AMDHS-22-78364 (R); Published: Nov 21, 2022, DOI: 10.5530/amdhs.2022.3.10
Abstract
Introduction: The currently available methods of fertility preservation for patients with breast cancer include cryopreservation of embryos, oocytes, and ovarian tissue and GnRH agonist treatment during chemotherapy. As the number of women who wish to become pregnant after being diagnosed with breast cancer increases, it is necessary to consider fertility preservation in these patients. However, medical doctors may be unaware of the importance of fertility preservation among cancer patients because most patients do not share their concerns about fertility with their doctors.
Objective: To assess the techniques for fertility preservation in patients with breast cancer-a current approach.
Materials and Methods: We performed a retrospective chart review of the cases of the 275 patients < 45 years old at the time of their breast cancer diagnosis at our institution during the period from January 2017 to December 2021 in Fertility Centre, Labaid Specialized Hospital, Dhaka, Bangladesh. Seventeen (6%) of the 275 patients decided to preserve their fertility before starting adjuvant systemic therapy. The collected data included patient age at the time of diagnosis, pathological diagnosis, the number of children the patient had at the time of diagnosis, tumor histology, nuclear grade, hormone receptor and human epidermal growth factor 2 (HER2) status, Ki-67 positivity, cancer stage, treatment regimens and duration, fertility preservation methods, number of successful pregnancies, and breast cancer recurrence. All data were retrospectively extracted from our institution’s electronic medical records system.
Results: 66 (24%) patients were single, 183 (66%) were married, and 26 (9%) were divorced. Of the 183 married patients, 24 (13%) had one or more children and 159 (87%) had none. All 26 divorced patients had one or more children. 72 (32%) patients received fertility counseling from the multidisciplinary team. Of the 72 patients given fertility counseling, 34 (47%) were single, 35 (49%) were married, and 3 (13%) were divorced. Of the 35 married patients who underwent fertility counseling, 13 (37%) already had one or more children and 22 (63%) were childless. 6 (35%) patients underwent oocyte cryopreservation, and 11 (65%) married patients opted for embryo cryopreservation. There were no pregnancies among the patients undergoing oocyte cryopreservation, whereas 3 (27%) of the patients who opted for embryo cryopreservation became pregnant. 2 (12%) patients stopped endocrine therapy after 2 years in an effort to become pregnant, but their breast cancers recurred.
Conclusion: Our present study focused on the importance of discussing fertility preservation with breast cancer patients. Patients with malignant diseases other than breast cancer such as leukemia, lymphoma, skin cancer, ovarian cancer, and sarcoma who may be treated by chemo- therapy, surgery or radiation therapy should also be considered. Though the problem of fertility loss for breast cancer patients is important and we should assess the infertility risk for all patients, we should also consider the prognosis.
https://betsatgirisi.com https://bettilte.com https://vegabete.com https://kanyongiris.com https://matgiris.com https://celtabetegiris.com https://hilbetegiris.com https://melbete.com https://kinbettinge.com https://wipbett.com https://pusulabetegiris.com https://superbahiss.com https://lidyagiris.com https://holiganbete.com https://1xbetgiriss.com https://asyabahise.com https://jetbahise.com https://betdoksana.com https://betebetle.com https://betgramagiris.com
Keywords
Fertility preservation, Multidisciplinary, Breast cancer, Young patients
Introduction
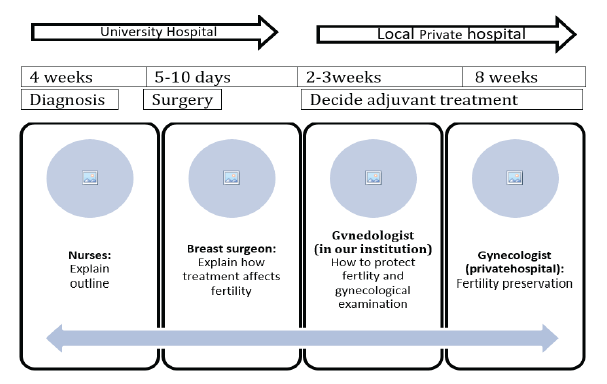
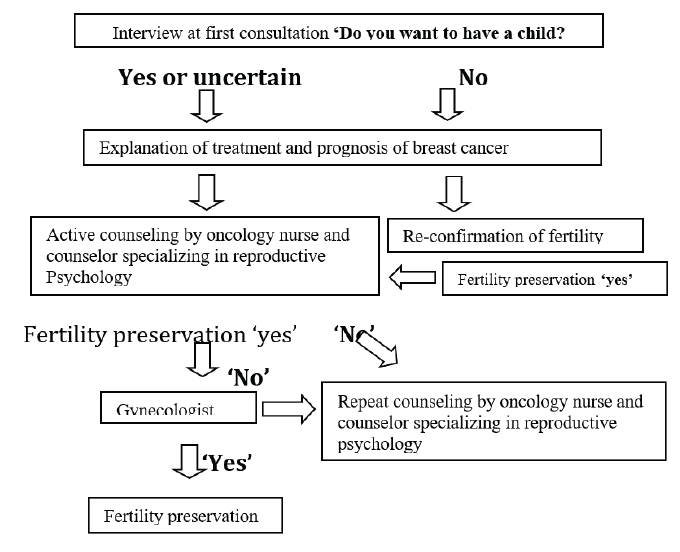
Breast cancer is the most common malignancy in women and a considerable amount of cases are detected during their reproductive life. The implications of breast cancer in young women (disease aggressiveness with need for systemic therapy in most cases, high five-year survival rate) and current trends in family planning in developed countries (deliberate delay of pregnancy until the late 30s or early 40s) make fertility preservation a necessary issue to attend to at the time of diagnosis. Recent improvements and growing research in fertility preservation techniques have made a number of possibilities available for these women. Breast cancer is one of the most common cancers affecting women worldwide. Thousands of young women are diagnosed with breast cancer every year [1,2]. Over the past four decades as diagnostic and treatment strategies (including surgery, irradiation and systemic therapy) have improved, the long-term out- comes of breast cancer patients have also improved [3]. Many patients with breast cancer can thus expect to live for many more years, and this progress raises important of quality-of-life issues such as fertility, which is particularly important for younger breast cancer patients [4,5]. Certain treatments for breast cancer, including chemotherapy and endocrine therapy, may adversely affect fertility [1,6]. Breast cancer treatment can have significant side effects including a transient or permanent impairment of gonadal function and subsequent infertility [7]. The duration of adjuvant endocrine therapy may also influence the timing of pregnancy for breast cancer patients. Five years of adjuvant endocrine therapy have traditionally been recommended, and treatment periods as long as 10 years have been recommended for patients with hormone receptor-positive cancers [8]. The potential adverse impacts of treatment on fertility can be a significant problem for younger breast cancer patients [9]. Many women diagnosed with breast cancer are concerned about the effects that cancer treatment may have on their fertility [9,10]. Ruddy et al. reported that almost half of their series of 620 breast cancer patients were concerned about becoming infertile after treatment, and their retrospective study of fertility concerns revealed that fertility preservation strategies were desired by young women with breast cancer [11]. However, there have been very few prospective studies on the current state of breast cancer patients’ attitudes or on how fertility preservation impacts the outcomes of these patients, and the efficacies of the available fertility preservation strategies remain poorly understood [12]. Since April of 2009, we (at Okayama University Hospital) have referred such relatively young patients for fertility counseling with a multidisciplinary team including a gynecologist, nurses and a counselor, and we have both considered and resolved the problems pertaining to the management of fertility issues (FIGURE 1 and FIGURE 2). We conducted the present study to evaluate the efficacy and safety of our current fertility preservation approach.
Materials and Methods
We performed a retrospective chart review of the cases of the 275 patients < 45 years old at the time of their breast cancer diagnosis at our institution during the period from January 2017 to December 2021 in Fertility Centre, Labaid Specialized Hospital, Dhaka, Bangladesh. The collected data included patient age at the time of diagnosis, pathological diagnosis, the number of children the patient had at the time of diagnosis, tumor histology, nuclear grade, hormone receptor and human epidermal growth factor 2 (HER2) status, Ki-67 positivity, cancer stage, treatment regimens and duration, fertility preservation methods, number of successful pregnancies, and breast cancer recurrence. All data were retrospectively extracted from our institution’s electronic medical records system.
Results
■ Patient characteristics
66 (24%) patients were single, 183 (66%) were married, and 26 (9%) were divorced. Of the 183 married patients, 24 (13%) had one or more children and 159 (87%) had none. All 26 divorced patients had one or more children. 72 (32%) patients received fertility counseling from the multidisciplinary team. Of the 72 patients given fertility counseling, 34 (47%) were single, 35 (49%) were married, and 3 (13%) were divorced. Of the 35 married patients who underwent fertility counseling, 13 (37%) already had one or more children and 22 (63%) were childless (TABLE 1).
| Marital Status | N (%) | Child | Counseling | Fertility preservation | Pregnancy/Giving-birth | Childrens age | |
|---|---|---|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | ||||
| Single | 66 | - | 34 | 7 | 0 | - | |
| (66/275, 24%) | - | (34/66, 51.1%) | (7/66, 10.6%) | 0% | - | ||
| Married | No Children | 24 | 13 | 7 | 2 | #1 | |
| 183 | (24/183, 13%) | (13/24, 54%) | (7/24, 29%) | (2/24, 8%) | 2 years old | ||
| (183/275, 66.5%) | ≥ 1 child | 159 | 22 | 3 | 1 | #2 | |
| (159/183, 87%) | (22/159=14%) | (3/159, 2%) | (1/159, < 1%) | 1 year old | |||
| Divorced | No Children | 3 | 0 | 0 | 0 | ||
| 26 | (3/26, 12%) | 0% | 0% | 0% | |||
| 26 (26/275, 9.4%) | ≥ 1 child | 23 | 3 | 0 | 0 | ||
| (23/26, 88%) | (3/23, 13%) | 0% | 0% | ||||
| Total | 275 | 72 | 17 | 3 | |||
| (72/277, 26%) | (17/277, 6%) | (3/277, 1%) |
■ Breast cancer patients with fertility preservation
Of all 275 patients, 17 (6.1%) decided to preserve their fertility after counseling. Six (35%) patients underwent oocyte cryopreservation, and 11 (65%) of the married patients opted for embryo cryopreservation. The single patients preserved their oocytes, and the married couples underwent embryos preservation. At the time of diagnosis, 7 patients were single and underwent counseling for fertility preservation. One patient got married after receiving the diagnosis and then decided to undergo embryo preservation after her marriage. Ultimately, 6 patients underwent oocyte cryopreservation.
Thirteen (76%) patients received adjuvant chemo-therapy. The 13 (76%) patients with Estrogen Receptor (ER)-positive breast cancer were given adjuvant endocrine therapy, and nine (53%) patients underwent both adjuvant chemotherapy and adjuvant endocrine therapy after fertility preservation. There were no pregnancies among the patients who underwent oocyte cryopreservation; whereas 3 (27%) patients with ER-negative breast cancer who opted for embryo cryopreservation became pregnant at > 2 years after the primary operation. Almost all of the ER-positive patients continued endocrine therapy, but 2 (12%) patients stopped endocrine therapy after 2 years in order to try to become pregnant, but their breast cancers recurred. There were 3 (18%) patients who opted to preserve fertility despite distant or local recurrence. The other 2 patients with local recurrence who discontinued endocrine therapy had been undergoing endocrine therapy for 5 years (TABLE 2).
| Case | Age | Marital status | Type of preservation | Timing of preservation | Pathology | Adjuvant treatment | Pregnancy | Recurrence |
|---|---|---|---|---|---|---|---|---|
| 1 | 35 | Single | Egg | POM1 | T2N0 G3 | TC→TAM | ||
| ER+/HER2- | ||||||||
| 2 | 32 | Single | Egg | POM1 | T2N3 G2 | AC→T→TAM | ||
| ER+/HER2- | ||||||||
| 3 | 35 | Single | Egg | POM2 | T1N0 G2 | TC→TAM | ||
| ER+/HER2- | ||||||||
| 4 | 37 | Married, | Embryo | POM1 | TisN0 | TAM (2 years) | Pregnant | |
| no children | ER+ | |||||||
| 5 | 38 | Married, | Embryo | POM2 | T2N0 G3 | AC→T/H | Pregnant | |
| no children | ER-/HER2+ | |||||||
| 6 | 39 | Married, | Embryo | POM1 | T3N2 G1 | AC→T→TAM | Distant | |
| no children | ER+/HER2- | (2 years) | ||||||
| 7 | 34 | Married, | Embryo | POM1 | T2N1 G3 | AC→T→TAM | Local | |
| no children | ER+/HER2- | (2 years) | ||||||
| 8 | 36 | Single | Egg | POM1 | T2N1 G3 | AC→T/H | ||
| ER-/HER2+ | ||||||||
| 9 | 32 | Married, | Embryo | POM1 | T2N1 G3 | AC→T→TAM | Local | |
| no children | ER+/HER2- | |||||||
| 10 | 39 | Single | Embryo | POM1 | Bilateral isN0 | TAM | ||
| ER+ | ||||||||
| 11 | 33 | Single | Egg | POM1 | T1N0 G3 | AC→T | ||
| ER-/HER2- | ||||||||
| 12 | 36 | Married, | Embryo | POM1 | T2N0 G3 | AC→T | Pregnant | |
| ≥ 1 child | ER-/HER2- | |||||||
| 13 | 43 | Married, | Embryo | Pre-operation | T1N0 G2 | TAM | ||
| no children | ER-/HER2- | |||||||
| 14 | 35 | Married, | Embryo | POM1 | T2N1 G3 | AC→T→TAM | ||
| no children | ER+/HER2- | |||||||
| 15 | 39 | Married, | Embryo | POM1 | T1N0 G2 | TAM | ||
| no children | ER+/HER2- | |||||||
| 16 | 35 | Married, | Embryo | POM1 | T2N1 G3 | TC→TAM | ||
| no children | ER+/HER2- | |||||||
| 17 | 39 | Married, | Embryo | Pre-operation | T1N0 G2 | TC→TAM | ||
| ≥ 1 child | ER+/HER2- |
Discussion
In this case series study, we evaluated the outcomes of our current multidisciplinary approach to fertility preservation for breast cancer patients. Breast cancer treatment can have significant side effects including a transient or permanent impairment of gonadal function and subsequent infertility [7]. Most chemotherapeutic agents damage the growing cells in mature and immature follicles, depending on the type of drug, the dose, and the age of the patients and this may result in the depletion of many or all follicles. For breast cancer treatment, we have usually used alkyl acting agents, including cyclophosph-amide, but these agents are quite toxic to the ovaries, particularly to the primordial follicles, which represent the ovarian reserve [13]. If the cancer is hormonal receptor-positive, the duration of adjuvant endocrine therapy may also influence the timing of the patient’s pregnancy. A high frequency of congenital abnormalities was reported to be related to the use of tamoxifen as the standard adjuvant endocrine therapy for premenopausal patients, before and during pregnancy [14]. Discussing the issue of fertility preservation is important for breast cancer patients who are of reproductive age and may want to have children [15,16]. Thus, all young patients should consider and discuss this issue with healthcare providers at the time that they are scheduled to begin the treatment. It is important for the healthcare provider team to recognize that patients may have concerns about fertility preservation. Breast cancer patients often lack adequate knowledge of issues pertaining to their reproductive functions at the start of treatment, and providing such information at the appropriate time allows the patient to select a treatment regimen without regrets [17]. Partridge et al. reported that 73% of younger breast cancer survivors had at least minor concerns, and 39% had major concerns about treatmentinduced infertility [10,18]. They also discussed awareness issues in a study showing that only 51% of breast cancer survivors were counseled about fertility preservation before starting treatment [10]. In our present series, only 26% of the patients received counseling for fertility preservation before starting breast cancer treatment. This rate was slightly lower than that reported by Ruddy et al.; their study also showed that concerns about fertility preservation are significantly affected by the social backgrounds of the patients and to vary among cultures worldwide [11]. As there have been no large prospective cohort studies focusing on this issue in Japan, we do not know whether our results reflect the social background of women in Japan. We thus need to plan a prospective cohort study with more patients. In our study, 6 (35%) patients underwent oocyte cryopreservation and 11 (65%), all of whom were married, opted for embryo cryopreservation. The 3 pregnancies in our cohort were all due to embryo cryopreservation. Most of the patients who did use fertility preservation techniques reported that they underwent embryo cryopreservation, the most efficacious of the widely available fertility preservation options. Oocyte cryopreservation, used by only 7 women in our cohort, is a newer technique that is generally offered to women who are unmarried [19]. The cryopreservation of ovarian tissue was also attempted [20,21]. It can be very difficult for breast cancer patients to consider and make a decision regarding whether they should undergo fertility preservation, given the prognosis of their cancer. It is therefore very useful for multidisciplinary team members to discuss this issue with the patient and her family. Two of the present 17 patients who underwent fertility preservation discontinued endocrine therapy after 2 years in order to try to become pregnant. Unfortunately, however, their breast cancers recurred. A previous study suggested that pregnancy after breast cancer does not negatively impact the disease outcome and is safe for the offspring: a large, multi- center, retrospective cohort study showed no difference in the disease-free survival rate between pregnant and nonpregnant patients with ER-positive breast cancer [22], and there was no difference in outcomes between the patients who did and did not become pregnant. The Breast International Group and the North American Breast Cancer Group launched a study to provide guidance for adopting customized strategies tailored to breast cancer patients wishing to become pregnant before completion of their entire course of adjuvant endocrine therapy. This trial, which is also evaluating the safety of pregnancy in breast cancer patients, is anticipated to provide answers for future generations of young women who wish to interrupt their endocrine therapy in order to try to have a baby [23]. Our present case series study has limitations, i.e., the small patient number due to the single-institute nature of the study, and the relatively short duration of follow-up. More data obtained from a larger number of patients and with longer follow-ups are needed. In conclusion, we evaluated the current approach to fertility preservation at our institution. Though the issue of fertility preservation for breast cancer patients is important and we should assess the infertility risk for all patients, we should also consider the prognosis of their breast cancer. However, this was a single-institute and retrospective study, and data from multicenter prospective cohorts allowing evaluations of the efficacy and safety of fertility preservation are currently lacking in Japan. Thus, in June 2016 we launched a prospective multicenter cohort study to evaluate the efficacy and safety of fertility preservation in greater detail. The population for the cohort is comprised of patients diagnosed with early breast cancer and registered as having undergone fertility preservation before the beginning of breast cancer treatment. We will collect the data of the outcomes of the fertility preservation and the breast cancer prognoses. The accrual goal is 50 patients for 5 years.
Conclusions
Our present study focused on the importance of discussing fertility preservation with breast cancer patients. Patients with malignant diseases other than breast cancer such as leukemia, lymphoma, skin cancer, ovarian cancer, and sarcoma who may be treated by chemotherapy, surgery or radiation therapy should also be considered. A discussion with a multidisciplinary cancer care team of how the treatment may affect a patient’s future fertility should be conducted before the patient begins her treatment.
References
- Goldfarb SB, Kamer SA, Oppong BA, et al. Fertility preservation for the young breast cancer patient. Ann Surg Oncol. 23(5), 1530-1536 (2016).
- Ferlay J, Soerjomataram I, Dikshit R, et al. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int J Cancer. 136(5), E359-386 (2015).
- Angarita AM, Johnson CA, Fader AN, Christianson MS. Fertility preservation: A key survivorship issue for young women with cancer. Front Oncol. 6, 102 (2016).
- Mayer EL, Gropper AB, Neville BA, et al. Breast cancer survivorsʼ perceptions of survivorship care options. J Clin Oncol. 30(2), 158-163 (2012).
- Vu JV, Llarena NC, Estevez SL, Moravek MB, Jeruss JS. Oncofertility program implementation increases access to fertility preservation options and assisted reproductive procedures for breast cancer patients. J Surg Oncol. 115(2), 116-121 (2017).
- Waks AG and Partridge AH. Fertility preservation in patients with breast cancer: Necessity, methods, and safety. J Natl Compr Canc Netw. 14(3), 355-363 (2016).
- Kim J, Turan V and Oktay K. Long-Term Safety of Letrozole and Gonadotropin Stimulation for Fertility Preservation in Women With Breast Cancer. J Clin Endocrinol Metab. 101(4), 1364-1371 (2016).
- Davies C, Pan H, Godwin J, et al. Long-term effects of continuing adjuvant tamoxifen to 10 years versus stopping at 5 years after diagnosis of oestrogen receptor-positive breast cancer: ATLAS, a randomised trial. Lancet. 381(9869), 805-816 (2013).
- Lambertini M, Anserini P, Fontana V, et al. The PREgnancy and FERtility (PREFER) study: an Italian multicenter prospective cohort study on fertility preservation and pregnancy issues in young breast cancer patients. BMC Cancer. 17(1), 346 (2017).
- Partridge AH, Gelber S, Peppercorn J, et al. Web-based survey of fertility issues in young women with breast cancer. J Clin Oncol. 22, 4174-4183 (2004).
- Ruddy KJ, Gelber SI, Tamimi RM, et al. Prospective study of fertility concerns and preservation strategies in youn women with breast cancer. J Clin Oncol. 32(11), 1151-1156 (2014).
- Shien T, Nakatsuka M, Doihara H. Fertility preservation in breast cancer patients. Breast Cancer. 21(6), 651-655 (2014).
- Jeruss JS, Woodruff TK. Preservation of Fertility in Patients with Cancer. N Engl J Med. 360(9), 902-911 (2009).
- Braems G, Denys H, De Wever O, Cocquyt V, Van den Broecke R. Use of tamoxifen before and during pregnancy. Oncologist. 16(11), 1547-1551 (2011).
- Duffy CM, Allen SM, Clark MA. Discussions regarding reproductive health for young women with breast cancer undergoing chemotherapy. J Clin Oncol. 23, 766-773 (2005).
- Thewes B, Meiser B, Taylor A, et al. Fertility-and menopause-related information needs of younger women with a diagnosis of early breast cancer. J Clin Oncol. 23(22), 5155-5165 (2005).
- Peate M, Meiser B, Friedlander M, et al. fertility-related knowledge, decision-making preferences, and treatment intentions in young women with breast cancer--an Australian fertility decision aid collaborative group study. J Clin Oncol. 29(13), 1670-1677 (2011).
- Howard-Anderson J, Ganz PA, Bower JE, Stanton AL. Quality of life, fertility concerns, and behavioral health outcomes in younger breast cancer survivors: A systematic review. J Natl Cancer Inst. 104(5), 386-405 (2012).
- OOCYTE M. Mature oocyte cryopreservation: A guideline. Fertil Steril. 99(1), 37-43 (2013).
- Shien T. Fertility concerns and preservation strategies in young women with breast cancer. J Thorac Dis. 6(6), 581-583 (2014).
- Fabbri R, Vicenti R, Magnani V, et al. Cryopreservation of ovarian tissue in breast cancer patients: 10 years of experience. Future Oncol. 8(12), 1613-1619 (2012).
- Azim HA Jr, Kroman N, Paesmans M, et al. Prognostic impact of pregnancy after breast cancer according to estrogen receptor status: A multicenter retrospective study. J Clin Oncol. 31(1), 73-79 (2013).
- Pagani O, Partridge A, Korde L, et al. Pregnancy after breast cancer: If you wish, maʼam. Breast Cancer Res Treat. 129(2), 309-331 (2011).